
Dial Osteotomy

TSUJI ORTHOPAEDIC INSTITUTE
PAINFUL LESIONShunichi Tsuji, M.D.
For preventing such disasters, dial osteotomy is a good solution. The acetabulum is cut like the ball shape and turned around over the femoral head like you are dialing the old style telephone.
Looking at the osteotomy of the pelvis (pelvic osteotomy), the results are not yet completely satisfactory with the conventional osteotomies. I think you know that those patients that had got operations for their hips previously may often have to get another one or end up with total hip arthroplasty. Our feeling in Japan is that unless there is remaining congenital dislocation of the hip, we can wait until the patients develop pain over their hips, thigh and sometimes over the knees at their adolescent age or thereafter. At this time we make a dial osteotomy of the acetabulum and the results are excellent if they meet the criteria below.
My indication for excellent results (90 to 95% excellent to good rates) includes:
1. Patients with painful hip joint between the ages seventeen and thirty-five.
2. CE angle of Wiberg between 0 and 20 degrees with no joint space narrowing.
3. Completely spherical femoral head with good joint congruity.
The fair to failure rates will increase up to 20 to 40% if you operate on patients who don't meet the above criteria depending on the age and the the stage of the osteoarthritic changes and coxa plana.
Here is what we do or you may want to do. Although there are some variations in the approaches and the method of osteotomy and bone graft, they are essentially the same. The most important point is to make a truly spherical osteotomy of the acetabulum around the femoral head half an inch extra-articularly. Dr. Mears at the University of Pittsburgh was kind enough to invite our colleague Dr. Sawaguchi from University of Kanazawa. Dr. Mears is a very excellent surgeon for the treatment of the fracture of pelvis. He was approaching the pelvis trans-trochanterically with his Mercedes incision for the treatment of pelvic fracture. I engaged in Dr. Sawaguchi's operations often and found that upper half of his approach that is Ollier's incision could be enough for dial osteotomy of the hip. This was good enough. Some surgeons in Japan make two skin incisions (Smith-Petersen and Southern approach) or make one big anteriorly convex skin incision and approach the hip joint anteriorly and posteriorly inside the same way. But using any approach you like, you can go over to the next procedure.

This is the traditional approach with one big anteriorly convex skin incision and two internal anterior and posterior incisions inside over the fascia like Smith-Petersen and Southern approach.


This is my favorite choice with Ollier's skin incision approaching the hip joint trans-trochanterically. This is the MIS Dial Osteotomy and
the patient can get on the wheel chair four days post-operatively for personal hygiene.

 For the osteotomy, you need special gouges (curved osteotomes) for the surgery. The radius of the gouge is two inches, the width is half an inch and the length is two inches (middle of three in the photograph). This is excellent for Japanese women but you may want ten to fifteen percent larger one for Caucasian woman or especially if the patient is male whose population is one tenth of the number female patients. In recent operations, I start the proximal cut half the diameter of the femoral head proximally from the joint space as you see in the one after next x-ray from here. Be careful not to come too close to the joint space because necrosis or collapse may develop in older patients with heavy body weight when you make the osteotomized acetabular fragment too small or too thin. Then you make the posterior cut. Be sure to find the greater sciatic notch visually or manually where the sciatic nerve exists, and start the cut right between the notch and the posterior rim of the acetabulum right on top of dorsum ischii (=posterior column). You may want to decline the handle of the gouge thirty degrees posteriorly and never damage the sciatic nerve.
For the osteotomy, you need special gouges (curved osteotomes) for the surgery. The radius of the gouge is two inches, the width is half an inch and the length is two inches (middle of three in the photograph). This is excellent for Japanese women but you may want ten to fifteen percent larger one for Caucasian woman or especially if the patient is male whose population is one tenth of the number female patients. In recent operations, I start the proximal cut half the diameter of the femoral head proximally from the joint space as you see in the one after next x-ray from here. Be careful not to come too close to the joint space because necrosis or collapse may develop in older patients with heavy body weight when you make the osteotomized acetabular fragment too small or too thin. Then you make the posterior cut. Be sure to find the greater sciatic notch visually or manually where the sciatic nerve exists, and start the cut right between the notch and the posterior rim of the acetabulum right on top of dorsum ischii (=posterior column). You may want to decline the handle of the gouge thirty degrees posteriorly and never damage the sciatic nerve.
The last osteotomy you want to make is the proximal portion of the ramus of pubis (=anterior column). For this purpose, many surgeons want to detach the origin of the rectus femoris from anterior inferior iliac spine (AIIS). They usually want to make a better view of the anterior column and also turning around the AIIS along with the rotating fragment of the bone. What I prefer to do is to osteotomise just proximal to the AIIS, thus leaving the rectus femoris where it is. But when you leave the rectus femoris where it is, you cannot see where you are going to start the cut on the proximal part of the ramus of pubis. I touch and feel the iliopsoas muscle and I start the cut just lateral to that muscle, in another words, closer to the anterior rim of the acetabulum. When you make this osteotomy, you may want to decline the handle of the gouge twenty-five degrees anteriorly.
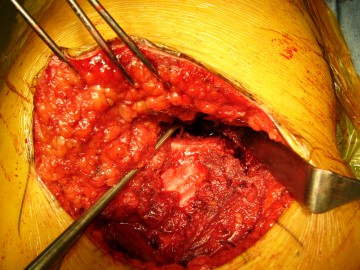
Using the bone hook the acetabulum is easily pulled over the femoral head.
Spherical rotation to any direction is easily possible.
Originally, they have had up to 2,000ml of blood loss at the time of surgery. But you can minimize it by keeping the patient's blood pressure somewhere between eighty and eighty-five millimeter of mercury during surgery and experiences of the physician shorten the time of surgery, thus you can do that with less than 400ml of blood loss. By means of preoperative blood storage, you do not have to make blood transfusion in most cases.
The dial osteotomy is called "rotational acetabular osteotomy" in Japan.
Recent Osteotomy Line:
In 1975, Eppright wrote the paper on JBJS about dial osteotomy of the acetabulum and he made the osteotomy just 1cm away from the articular cartilage. This is technically demanding and carries a high risk of perforating into the joint line with which alleviation of hip pain is no more expected any longer.
In 1978, Wagner described about spherical acetabular osteotomy for the correction of the dysplastic acetabulum in a book. He used a spherical chisel. I have never used his chisel and I guess it might be difficult to pull out after the first insertion into the pelvis at the time of osteotomy, because the same thing happens with our chisel. Even though it is hard to remove, it is far better to make the first osteotomy deep into the pelvis, so that we can prevent fragmentation of the osteotomized acetabulum which is thin medially.
In 1982, Ninomiya wrote papers on rotational acetabular osteotomy (RAO) in Japanese and subsequently in 1984 in English on JBJS. We are basically doing the similar osteotomy with some modifications.
In December 1984, I had a chance to attend the AO course at Davos, Switzerland. At that time, Swiss doctors taught us about the Ganz osteotomy. They said Herr Professor Ganz (Reinhold Ganz) at University of Bern is a genius surgeon and only he can do this operation in the whole world (in der ganzen Welt!). He wrote the paper on Clin Orthop in 1988 and his osteotomy line is more away from the acetabular cartilage than our osteotomy line but similar except that they approach from inside the pelvis. This is prevailing in the United States as Bernese periacetabular osteotomy (PAO) nowadays.
In 1989, Hasegawa at Nagoya University started eccentric osteotomy. The center of rotation is proximal and lateral so we need no bone graft and we can bring the somewhat subluxated femoral head medially like the rotor in the rotary engine from Mazda. I will show you the osteotomy line by Ninomiya (green line) and my preferens (red line) for eccentric rotation. I also cut at green line if the patient has a shallow hip socket. The osteotomy at red line is more difficult but when the patient asks me after complete recovery if she can have a natural normal delivery and I can answer "Yes." without any hesitation. Of course they don't need to undergo Caesarian section even if you cut at green line. Let me mention, in addition, our approach does not affect the infertility rate. We usually recommend the patient to get the operation before giving birth to babies in order to avoid deterioration of osteoarthritic changes during pregnancy and while carrying babies. And also mothers can stay with the babies after birth all the time keep taking care of them without interruption by their own operation.
The AP, PA, lateral, superior and inferior views are as follows.
 AP
AP
 PA
PA
 Lat.
Lat.
 Med.
Med.
 Sup.
Sup.
 Inf.
Inf.
For getting easier image, the circumferential views are as follows.

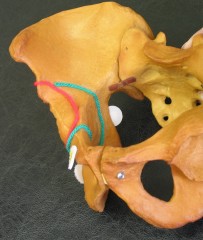








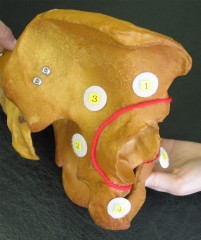
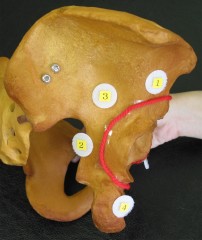




Ninomiya taught us to start the osteotomy one finger breadth proximal from acetabular rim and I measured my index finger and "1 fb" was 18mm for me.(^_^) For preventing collapse of the osteotomized acetabular fragment, now I start osteotomy 22 to 23mm away from the joint line. The numbers in the photos show the order of osteotomy which I prefer to do.
Advantages of Dial Osteotomy over the Periacetabular Osteotomy:
#1. With the dial osteotomy, it is possible to make a good coverage of femoral head not only superiorly but also posteriorly as well because it's a completely free spherical rotation with no limitation to find the place to fix the bone with. (In that term, the name of the osteotomy may have to be "Spherical Osteotomy" instead of "Dial Osteotomy".) This kind of rotation is important because there also exists a developmental dysplasia posteriorly at the posterior column of the acetabulum. You can see this rotation in my recent operation here. The two-dimensional AP x-ray appearance just gets better only when the AIIS is rotated laterally at the superior portion of the femoral head. But the superior area around the AIIS is narrow and small in patients with DDH and not enough for weight-bearing all alone, and the smaller area of femoral head coverage will lead to the future failure. The most important place to cover is the area around the posterior column where the weight-bearing area is wide and rigid along with the superior area coverage as well. Note that already less developed part of posterior column of acetabulum with DDH is further medially rotated with PAO. It is important to think about the rotation three-dimensional wise. Two-dimensional x-ray or c-arm image intensifier guide is very helpful but not satisfactory enough. It is important to put the rotating acetabulum under direct visualization and make a three-dimensional complete correction.
#2. We do not go inside the pelvis, so there is no worry about increase of infertility rate and the increased choice of caesarean section by the obstetrician even without the presence of placenta praevia, breech presentation, or previous history of c-section.
References:
1. Eppright, RH: Dial osteotomy of the acetabulum in the treatment of dysplasia of the hip. J Bone Joint Surg, 57A: 212-214, 1975.
2. Wagner H. Osteotomy for congenital hip dislocation. In:The Hip. The C.V. Mosby Company, Saint Louis 1976: 45-66.
3. Wagner H. Experiences with spherical acetabular osteotomy for the correction of the dysplastic acetabulum. In: Wei UH, editor Progress in orthopaedic surgery. Vol 2. Acetabular dysplasias in childhood. New York: Springer; 1978: 131-145.
4. Ninomiya, S; Tagawa, H: Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg, 66A: 430-436, 1984.
5. Ganz, R; Klaue, K; Vinh, TS and Mast, JW: A new peri-acetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop, 232: 26-36, 1988.
SITE MAP
#HOME-Dedication
#PAINFUL LESION
-Osteoarthritic Knee-Minimally Invasive Total Knee Arthroplasty(Full Flexion Knees)-10yr. F/U-Intra-Op. Photo
-Osteoarthritic Hip-THA(Video movie)-Cemented THA-Minimally Invasive Total Hip Arthroplasty
-Acetabular Dysplasia-JSN-Acute Destruction-Dial Osteotomy-8yr. P.O.-Recent Development
-Humeral Head Fracture-DJD Shoulder-Humeral Head Prosthesis
-Cuff Tear Arthropathy-RCT-Cuff Repair
#TOUR
-Minneapolis-Sears Tower-Skyscrapers-Stream of Lights-Niagara Falls-The Lady-U of M-OR-Mt. Rushmore-AAOS-LA from Hollywood-Walt Disneyland-Grand Canyon-Downtown Minneapolis-Kind Doctor-Linda
#LOCATION(Location-Map by Its-mo Guide Map by MapFan)